
Complete care coordination is a comprehensive approach to case management in addiction recovery that includes long-term support, professionally coordinated cultures of enthusiastic peer recovery and family support, and a goal of achieving long-term recovery. It is designed to give individuals the best possible chance of achieving sustained long-term recovery by providing continuous support and coordination across the entire recovery journey, including during relapse periods. Complete care coordination is distinguished from traditional care coordination, which is limited in duration and only takes place during the early stages of sobriety.
Definitions
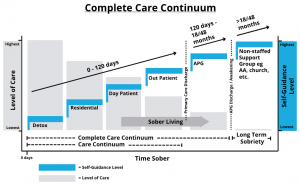
Care coordination traditionally accepted by the recovery industry refers to case management that includes a minimum of one of three main types of professional communication executed within the care continuum (see the diagram below) for the benefit of the recoveree during early recovery. The three main types of communication are: 1) between organizations during a recoverees transitions from one level of care to another, 2) between staff within a single organization, and 3) between staff and stakeholders, like family, involved in a client’s recovery. Unfortunately, traditionally accepted care coordination is limited in its duration as it takes place solely within the very beginnings of early sobriety e.g. primary care (0-120 days). Occasionally, some sober living homes (6-9 months) work to extend some level of care coordination. Although despite that occasional extension, both primary care and sober living’s care coordination fall short of helping recoverees achieve robust long term sobriety.
Complete Care Coordination, on the other hand, is much more than simple care coordination. Yes, care coordination is a part of Complete Care Coordination but Complete Care Coordination is a higher fidelity of care coordination. It is a process that includes long term case management, professionally coordinated cultures of enthusiastic peer recovery and family support, and the goal of achieving long term recovery. Additionally within Complete Care Coordination, each component of early recovery care coordination takes place simultaneously and continuously across the entire recovery lifespan, including relapse periods, until long term sobriety is achieved no matter how long that takes. Complete Care Coordination is known as ‘complete’ because research indicates it gives recoverees the best possible chance of achieving sustained long term recovery.
Levels of Care
In the addiction recovery process, there are various levels of care a recoveree can go through. Starting at the highest level of care and stepping down gradually is detox, residential, day patient, out patient, and APG (alternative peer group). The ultimate goal is of course building up a recoveree’s esteem, resilience, and resources to the point they can achieve long term sobriety and maintain it without needing any level of professional care. However, each person’s recovery journey and treatment plan is unique. They all do not have to start at the same level of care or even progress through each level in a systematic step wise fashion as detailed in the chart below. For example, some recoverees may jump straight from detox to out patient while others may start with day patient and transition directly into an APG after discharge. Furthermore, addicts do not all recover at the same rate and have varying amounts of sobriety attempts stretched out over different lengths of time. Their reaching long term sobriety is marked by enough time having passed for their brain neurology to have healed, positive life affirming behaviors to have taken root and habitually replaced negative destructive ones, and their chances of relapse having been significantly minimized.
Below is a chart detailing the complete recovery journey aka the Complete Care Continuum from the highest level of care to the lowest. It also illustrates the inverse relationship between the level of care and level of self-guidance. In other words, as one decreases, the other increases.
Limitations of Care Coordination
Prior to the achievement of long-term sobriety (18-48 months), recoverees are traditionally left without professional care and accountability causing a giant treatment gap, opening the door for program hopping, inhibiting Complete Care Coordination, and risking unnecessary relapse.
When all the levels of care a recoveree goes through are not conducted under the same roof and do not communicate with each other during transitions from one level of care to the next or when bridging sobriety attempts across time, problems can arise. When that happens, treatment gaps and program hopping can occur that undermine a recoveree’s chances for success. Treatment gaps occur within a single organization due to a lack of coordination amongst staff. Additionally, gaps occur if an organization’s staff and client recovery stakeholders, such as family, become out of sync, miscommunicate, or simply just do not talk to each other.

Successfully discharging from primary care treatment (0-120 days) and joining an unstructured, non-professionally staffed support group is only just a start at defending against relapse. Although by itself, it is actually an incomplete defense. Recoverees need a healthy, structured environment to grow within that offers encouragement, accountability, and fun while simultaneously offering family support and Complete Care Coordination. Non-professionally staffed support groups, such as AA, are not set up to offer professional oversight or coordination. A group like AA is a great but it’s effectiveness on getting higher percentages of recoverees to long term sobriety is limited by its fellowship structure.
It is true that if a recoveree is gung ho about being sober and can maintain the enthusiasm and pro-activity necessary to achieve long term sobriety, they can make it with just AA. The problem is the statistics say that that is most often not the case as enthusiasm usually is short lived, negatively effecting pro-action. Without a structure of encouragement, accountability, and social fun, relapse is almost inevitable. In fact, around 50% of recoverees who complete primary care left to their own devices and are given the suggestion to continue their program on their own, including attending AA meetings, relapse within the first 90 days after discharge. Attempting recovery without having the goal of achieving long term sobriety is basically gambling with your loved ones life as there is never a guarantee a recoveree will return to attempt sobriety again. Unfortunately, many don’t make it back and pass on to the next world before a successive attempt ever happens. (Contact us if you need to talk to a veteran Lifeway staff member who has been to entirely too many funerals due to this deadly disease.)
The Complete Care Coordination Advantage of the APG Model
In response, alternative peer groups proactively address these issues head on by systematizing communication between organizations during client movement from one level of care to the next, by linking a client’s recovery experience together as a single continuous journey, and by conducting regular progress updates between staff members and stakeholders. Not only do regular and proactive communications drive positive recovery outcomes, but over the journey to long term sobriety they also create the deepest and most robust understandings of the uniqueness of a client’s story, character, and relationships. Short term solutions simply fall short.
For recoverees, what is much more often the norm is needing professional care, peer reinforcement, and family support that can guide them on their way to trudging the road of happy destiny. If/when they achieve long term sobriety, their chances of continuously making it are far, far greater. In fact, a study done at Baylor College of Medicine found >80% of recoverees who successfully completed an APG outpatient program and stayed active in an APG went on to achieve a minimum of 2 years of sobriety. While another, 15 year study conducted by the same research team found 74.1% of recoverees who stayed highly active in an APG were still sober at 5 years out. Furthermore, The Recovery Research Institute of Massachusetts General Hospital, an affiliate of Harvard Medical School, dedicated to the advancement of addiction treatment and recovery, defines 5 years of continued remission as ‘the point at which the risk of meeting criteria for a substance use disorder in the following year is no greater than that of the general population’.
The Optimal View
The APG model is the last, though sometimes only, level of professional care a client goes through prior to achieving long term sobriety as well as where information from all previous levels of care flows. As such, Lifeway is optimally positioned to oversee and manage the entire treatment process with Complete Care Coordination from a recoveree’s first day to their successful realization of long term sobriety.
In addition, Lifeway is structured so all staff members who directly interact with a client are in constant communication with each other and can operate collectively from the same page as a single voice. Client staff members take responsibility for keeping up with what is going on with their clients and their client’s family during treatment. No matter what level of care the client is receiving, staff stays plugged-in in order to quickly respond to newly arising issues and catch critical details that might otherwise have fallen through the cracks until the goal of long term sobriety is achieved.
Proactive Linkages and Avoiding Program Hopping
When a client becomes a part of Lifeway, staff will proactively reach out to the client’s previous level of care in order to get a more accurate picture of their unique case and circumstances. When Lifeway clients regress in their recovery and subsequently need to return to a higher level of care, they will be referred back to the case manager at their original higher level of care in order to maintain strong recovery coordination and avoid inconsistencies due to program hopping. However, even if program hopping ends up happening despite advice, Lifeway still acts as a hub for client information and actively connects and coordinates with the client’s chosen higher level care. This kind of proactive linkage, as opposed to passively waiting, keeps a loving professional eye watching over the recoveree no matter where they go. Additionally, the progress updates help inform the Lifeway family counselor as to how to best serve the recoveree’s family while the client is completing higher level care.
Keys to Effective Complete Care Coordination
The key to Complete Care Coordination in recovery is it needs to be consistently conducted, uniformly applied, and persistently moving towards optimizing outcomes no matter how long the recovery journey takes. For example regarding the establishment of boundaries, if a client is met with the same responses from the same people for their actions, they will better come to understand and accept their boundaries while learning to function within them. However without continual reinforcement from peers, staff, and family, a client will figure out their boundaries can be stretched and bypassed when they are inconvenient to what they want. Consistent accountability from a recovery network of staff, stakeholders, and peers leads a client to cultivating wider acceptance of healthy boundaries.
Contact us for a Strategy Appointment and get plugged in with Complete Care Coordination.
Schedule a Strategy Appointment Today
Or if you’d like to learn more about the continuous journey of recovery, give us a call at (713) 459-9427 and we’ll be happy to answer your questions.

